HISTORY OF PRESENT ILLNESS:
* Patient was apparently asymptomatic 5 yrs back when he had pain abdomen & vomitings for which he was taken to a local hospital and treated conservatively.
* He continued taking alcohol, following which he had recurrent episodes of pain abdomen & vomiting
* 5-6 episodes in the past 1 year previously it was 1 episode in every 4 to 6 months , associated with weakness and Giddiness
*Last episode was 25 days ago , where he had multiple episodes of vomiting after consuming fish and rice , not associated with pain. Vomitings did not stop after taking oral medication, so the patient went to a hospital.
* Last binge of alcohol 6 months back following which he again had pain abdomen & vomiting .
* abdominal pain in umbilical, left hypochondriac, left lumbar and hypogastric regions.
* Abdominal pain was increased after food intake , Very severe type of pain interfering with daily activities
* Pain is throbbing type and radiating to the back and is associated with nausea and vomiting , which is non bilious, non projectile and has food and water as contents
*The pain would aggravate after consuming alcohol and fat-rich food, and relieved after getting admitted to the hospital(for 2-3 days), where he was given painkillers I.V. Initially the pain was not associated with vomiting but with fever
*For the past 6 months, the patient has been experiencing pain continuously every day, which did not resolve even on taking oral medication.
*Complains of weight loss around 15 kg in the past 6 months.
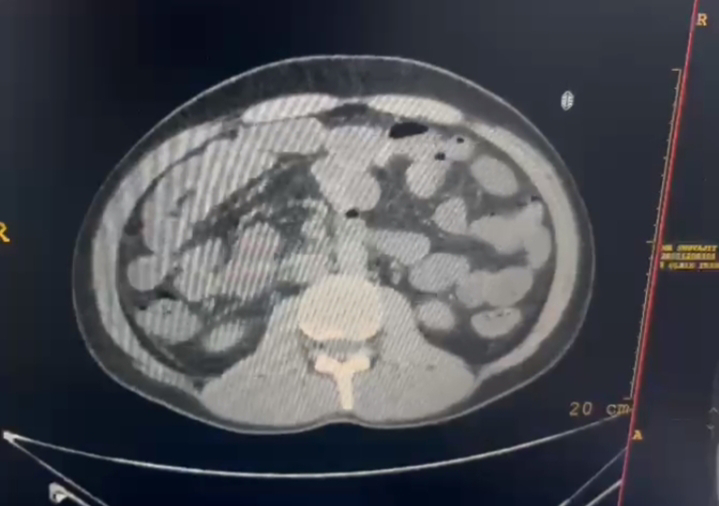
"In August 2022 ,the patient had an episode of abdominal pain and vomiting, for which he was admitted to a hospital. A CT of abdomen was performed and a lump was found in the pancreas. On further investigation, it was found that the lump was not cancerous. The patient was given symptomatic treatment and discharged when he was stable."
* Complains of Constipation,per rectal bleeding since childhood
*From the past 6 months, the patient also complains of severe pain in both the legs ( in the calf region ), below the knee, which developed after trauma . The pain would start while sleeping or sitting for a long time. It is muscular in nature. The pain would get reduced by massaging the area. The pain is so severe that he is not able to sleep. He does not get the pain while walking. It is not associated with any changes in the overlying skin or swelling or muscle cramps.
*History of depression and he is attending psychiatric counselling sessions now .
PAST HISTORY:
*He is Known case of haemorrhoids since the age of 12
*History of appendectomy
*History of leprosy 12 years ago
*He is a Know case of hypertension for past 5 years but not on any medication
* No history of diabetes mellitus, tuberculosis.
* No history of previous blood transfusions.
PERSONAL HISTORY:
The patient is prone to stress
*Sleep: Reduced sleep from 5 years,
Consumes medicines for sleep.
* Appetite: Normal
* Diet: mixed
* Bowel and bladder movements : Constipation since 25 years , associated with blood in the stools
* Additions:1) Alcoholic since 10 years , consumes 180 ml alcohol daily.
Stopped on alcohol since 6 months
*SMOKING- 2 packs a day from when he was in college. 1 pack a day from 6 months.
*ALLERGIES- no
**Daily routine: He wakes up at 6am in the morning , gets ready for work , takes breakfast , goes to the office ,completes his work and returns by 5pm and plays badminton or football and comes back home ,used to consume alcohol before or after dinner , takes dinner at 8pm and goes to bed by 10pm.
FAMILY HISTORY:
Not significant
GENERAL EXAMINATION:
Patient is conscious coherent and cooperative.
He is well oriented to time, place and person.
He is moderately built and moderately nourished.
VITALS:
Temperature: Afebrile
Pulse Rate: 86 beats per minute
Blood pressure: 120/90 mm of Hg (supine postion - left arm)
Respiratory Rate: 18 cycles per minute
SpO2: 95% on room air
GRBS : 128 mg/dl
No Pallor
Icterus present
No Cyanosis
No Clubbing
No Lymphadenopathy
No Edema
SYSTEMIC EXAMINATION:
1) Abdominal examination:
Inspection:
Shape of the abdomen: normal
Umbilicus: normal
* No visible pulsations
* All quadrants of abdomen are moving equally on respiration.
* Grey turner sign ( bluish discolouration of flanks) and Cullens sign( bluish discolouration of periumbilical area ) are negative [ These are +ve in patients with severe pancreatitis with Haemorrhage ]
Palpation:
* No local rise of temperature
* Slight Tenderness present over left hypochondriac region.
* Guarding and rigidity : present
* No palpable masses found
* Liver and spleen are not palpable
Percussion :
* Liver span: normal
Auscultation:
* Sluggish bowel sounds are heard.
2) Respiratory system:
Slight left side deviation of the nasal septum that developed after trauma ,which did not affect his daily life
* Bilateral Normal vesicular breath sounds are heard.
*Position of trachea : central
3) CVS:
* S1 and S2 heart sounds are heard
*No murmurs
4) CNS:
* No focal neurological deficits
Provisional diagnosis:
Acute on Chronic pancreatitis
( Stress, Depression)
INVESTIGATIONS:
* Imaging:
1) CE CT ( Contrast Enhanced CT):
Usg abdomen
X-ray Knee Joint


























Comments
Post a Comment