Medical case disscussion
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent
Here we discuss our patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs
This E log book also reflects my patient - centered online learning portfolio and your valuable inputs inthe comment box are welcome.
Name : Mounika 7th sem
Roll no : 46
I have been given this case to solve an attempt to understand the topic of "patient clinical analysis data " to develop my competency in reading and comprehending clinical data including clinical history,clinical findings, investigations and come up with a diagnosis and treatment plan
65 YO FEMALE WITH FEVER, ABDOMINAL PAIN AND SOB
65 year old female a resident of Suryapet got admitted to the hospital on 9/11/21 with the
●CHIEF COMPLAINTS of:
Fever since 4/11/21SOB since 5/11/21Abdominal pain since 5/11/21
●HOPI:
The patient started experienceing head ache on the evening of deepawali and later the same day also developed a fever that was low grade, was associated with chills and did not decrease on taking medication.
The next day she started developing shortness of breath, which was sudden in onset. It was progressive in nature initially she had SOB on doing her regulat house hold work ( Grade 2 NYHA ) which later progressed till she could not do even minimal activity ( Grade 3 NYHA ). It was not associated with orthopnea or PND. There was no diurnal variation.
On the same day she also developed Abdominal pain. It was in the upper part of the abdomen ( Right and left hypochondrium and epigastrium). It was prickling in nature and radiated to the left side of the chest and left axilla. It was associated with abdominal tenderness and distension.
No history of nausea, vomitings, diarrhoea, burning micturation.
The patient has tremors that reduce on movement that are intermittent in nature in her left hand for the past 4 years that has increased in frequency recently.
●PAST HISTORY:
No similar complaints in the past.
The patient is a known case of Hypertension for the past 8 years under medication (TELMA)
The patient was diagnosed with HTN when she went to a local hospital with complaints of neck swelling and pain.
Patient is not a known case of DM, TB, Asthama.
●PERSONAL HISTORY:
Diet: Mixed
Appetite: Normal
Sleep: Normal
Bowel: Regular
Bladder: Decreased urineation.
Habits: Does not consume any form of alcohol or tobacco.
●FAMILY HISTORY:
Not significant
●DRUG HISTORY:
TELMA for hypertension since the past 8 years.
●DAILY ROUTINE:
Until an year ago she worked as a daily wage labourer. Now she wakes up at 6 am. She has her breakfast at 7 am. Then does some household work. She then has lunch at 3 pm. Dinner at 8 pm and goes to bed at 9 pm.
●GENERAL EXAMINATION:
The patient was examined in a well lit room after obtaining consent.
The patient was conscious, coherent and cooperative. He was moderately built and moderately nourished.
Pallor: Absent
Icterus: Absent
Cyanosis: Absent
Clubbing: Absent
Lymphedenopathy: Absent
Edema: B/l pedal edema present of pitting type.
●SYSTEMIC EXAMINATION:
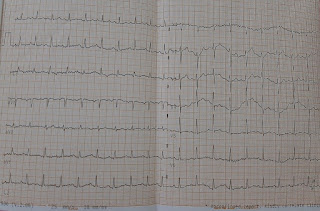
CVS:
Precordium is normal
Thrills absent
Precordial heave absent.
S1 and S2 heard.
No murmurs heard.
RS:
Chest is elliptical
Trachea: Central
Symmetrical expansion of chest.
Vesicular breath sounds heard.
No adventitious breath sounds heard.
ABDOMEN:
Abdomen is distended
Moves symmetrically with respiration
Umbulicus is central and inverted
No scars or sinuses
No local rise in temperature
Tenderness in the left hypochondrium and epigastrium.
No organomegally
CNS:
Higher mental functions normal.
Cerebellar functions normal.
Cranial nerve examination normal.
Sensory examination: decreased sensation of bilateral lower limbs.
Motor examination:
Power: upper limbs: 4- bilaterally
Lower limbs: 4 + bilaterally.
Tone: Normal
Reflexes:.
R L
Biceps: 2 2
Triceps: 2 2
Knee: - -
Ankle: - -
Tremors are seen.
Intermittent in nature.
●Investigations :
●X-ray chest :
No evidence of any free fluid noted in bilateral pleural cavities
No evidence of any consolidatory changes noted in bilateral lung fields
No sonological abnormality detected
Hb-10.5
TLC- 11000
PLC- 2.19 lakhs /cumm
RBC- 3.98 million/cumm
PCV- 30.8 vol%
MCV- 77.4 fl
MCH- 26.4 pg
MCHC- 34.1%
RDW-CV - 16.2%
RDW-SD - 46.1 fl
Smear :
RBC : NORMOCYTIC NORMOCHROMIC RBC
WBC : LEUCOCYTOSIS
PLATELETS : adequate in number and distribution
HAEMOPARASITES : not seen
IMPRESSION : NORMOCYTIC NORMOCHROMIC Anemia with mild LEUCOCYTOSIS
●Provisional diagnosis:
Acute kidney disease under evaluation








Comments
Post a Comment